The Effectiveness of a Machine Learning Model in Predicting Blood Transfusion Probability in Bipolar Hemiarthroplasty Hip Replacement Surgery
DOI:
https://doi.org/10.56929/jseaortho-2026-0287Keywords:
machine learning, fracture neck of femur, bipolar hemiarthroplasty, transfusionAbstract
Purpose: To verify a machine learning-based prediction model for blood transfusion risk in patients undergoing bipolar hemiarthroplasty and to determine whether there are significant differences between the accuracy results of this verification and the original model.
Methods: A retrospective study using purposive sampling was designed to gather 136 samples with the inclusion criterion of undergoing bipolar hemiarthroplasty for femoral neck fractures at the author’s institution between January 1, 2021, and June 30, 2024. The research instruments included (1) a machine learning-based prediction model for blood transfusion probability (smskbl.streamlit.app), which was constructed using 232 femoral neck fracture samples undergoing bipolar hemiarthroplasty at the author’s institution from 2015 to 2020, and (2) a research questionnaire created by the researcher, including six items: one on demographic data, four on medical health conditions, and one on actual blood transfusion during surgery.
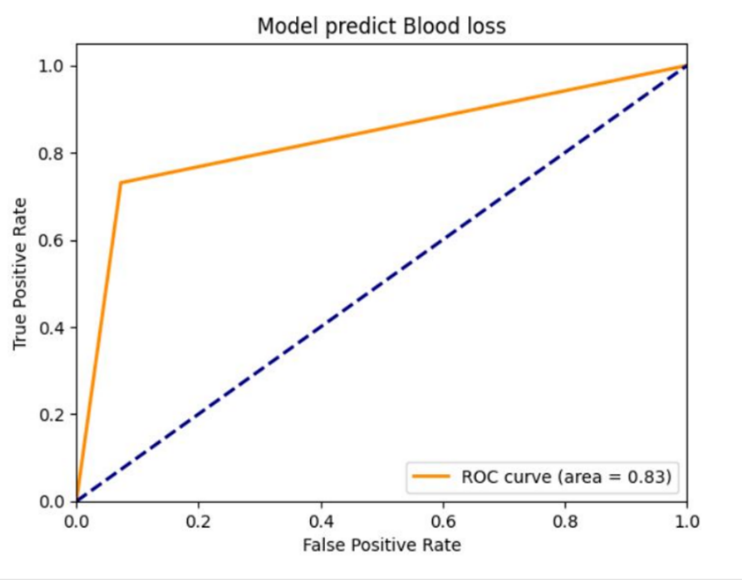
Results: The prediction model accuracy was 89%, compared with that of the original model (80%). The comparison of the accuracy results was not statistically significant (Z = 0.424, p > 0.05). In the blood transfusion group, the precision was 0.70, recall was 0.73, and F1-score was 0.72, whereas the group that did not receive blood transfusion had a precision of 0.94, recall of 0.93, and an F1-score of 0.93. The area under the curve was 0.83.
Conclusions: The blood transfusion prediction model demonstrated good performance in predicting transfusion risk. The model provides confidence in its risk prediction outcome and can be used to perform optimal risk management in preparation for bipolar hemiarthroplasty.
Metrics
References
Li X, Luo J. Hemiarthroplasty compared to total hip arthroplasty for the treatment of femoral neck fractures: a systematic review and meta-analysis. J Orthop Surg Res 2021;16:172.
Bisbe E, Basora M, Colomina MJ. Peri-operative treatment of anaemia in major orthopaedic surgery: a practical approach from Spain. Blood Transfus 2017 ;15:296-306.
Coccolini F, Shander A, Ceresoli M, et al. Strategies to prevent blood loss and reduce transfusion in emergency general surgery, WSES-AAST consensus paper. World J Emerg Surg 2024;19:26.
Harris JC, Crookston KP. Blood product safety. [Internet]. 2023 [cited 2025 Dec 5]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK539826/
Stoker AD, Binder WJ, Frasco PE, et al. Estimating surgical blood loss: A review of current strategies in various clinical settings. SAGE Open Med 2024;12:20503121241308302.
Müller MM, Geisen C, Zacharowski K, et al. Transfusion of packed red cells: indications, triggers and adverse events. Dtsch Arztebl Int 2015;112:507-17; quiz 518.
Zang H, Hu A, Xu X, et al. Development of machine learning models to predict perioperative blood transfusion in hip surgery. BMC Med Inform Decis Mak 2024;24:158.
Hendrix JM, Garmon EH. American Society of Anesthesiologists Physical Status Classification System. [Internet]. 2025. [cited 2025 Dec 5]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441940/
Guan J, Li Z, Sheng S, et al. An artificial intelligence-driven revolution in orthopedic surgery and sports medicine. Int J Surg 2025;111:2162-81.
İndelen C, Uygun Kızmaz Y, Kar A, et al. The cost of one unit blood transfusion components and cost-effectiveness analysis results of transfusion improvement program. Turk Gogus Kalp Damar Cerrahisi Derg 2021;29:150-7.
Liang D, Pang Y, Huang J, et al. Predicting postoperative blood transfusion in elderly patients undergoing total hip and knee arthroplasty using machine learning models. Risk Manag Healthc Policy 2025;18:1697-711.
Buddhiraju A, Shimizu MR, Subih MA, et al. Validation of machine learning model performance in predicting blood transfusion after primary and revision total hip arthroplasty. J Arthroplasty 2023;38:1959-66.
Luangwaranyoo A, Suksintharanon M, Tangadulrat P, et al. Factors for blood transfusions following hemi hip arthroplasty for patients with femoral neck fracture. Geriatr Orthop Surg Rehabil 2020;22;11:2151459320972993.
Santanapipatkul P. Machine learning risk factors for blood transfusion after hip arthroplasty in fracture neck femur patients. Region 4-5 Medical Journal 2021; 40:381-8.
Lalehzarian SP, Gowd AK, Liu JN. Machine learning in orthopaedic surgery. World J Orthop 2021;12:685-99.
Hamdi OA, Danan D, Denner A, et al. Impact of implementing stricter criteria for blood transfusion in patients with head and neck cancer undergoing free tissue transfer. Laryngoscope Investig Otolaryngol 2024;9:e70021.
Argov S, Shechter Y. Is routine crossmatching for two units of blood necessary in elective surgery? Am J Surg 1981;142:370-1.
Seong H, Lee KS, Choi Y, et al. Explainable artificial intelligence for predicting red blood cell transfusion in geriatric patients undergoing hip arthroplasty: Machine learning analysis using national health insurance data. Medicine (Baltimore) 2024;103:e36909.
Dziadkowiec O, Durbin J, Muralidharan VJ, et sl. Improving the quality and design of retrospective clinical outcome studies that utilize electronic health records. HCA Healthc J Med 2020;1:131-8.
Soldati S, Colais P, Davoli M, et al. More is more? The role of surgeon in the volume-outcome relationship: an Italian population-based cohort study. BMJ Open 2025;15:e098569.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2026 The Royal College of Orthopaedic Surgeons of Thailand

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.