Rates, Predictors of Blood Transfusion, And Changes of Hematocrit Level in Geriatric Hip Fractures
DOI:
https://doi.org/10.56929/jseaortho-2025-0261Keywords:
Hip fracture, Elderly, Blood transfusion, Hematocrit level, Hip fracture surgeryAbstract
Purpose: This study aimed to determine the prevalence and risk factors associated with blood transfusion in elderly patients with hip fractures, along with changes in hematocrit level during the first three days of hospitalization, to create more appropriate preoperative assessment guidelines.
Methods: Patients with intertrochanteric, femoral neck, and subtrochanteric fractures who underwent surgical treatment from May 1, 2021–April 30, 2023, were included. Multivariate analysis was used to identify predictors of blood transfusion. Changes in hematocrit level during the first three days of hospitalization were also calculated.
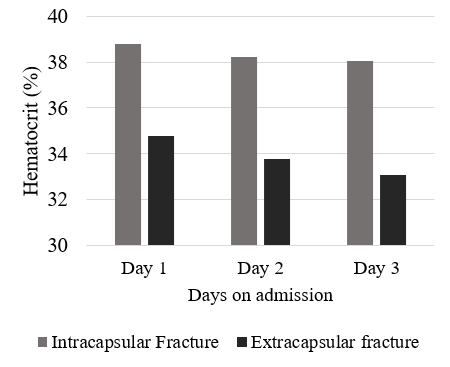
Results: Blood transfusion rate among elderly patients with hip fractures who underwent surgery was 43.12%. Multivariable analysis identified three significant risk factors for transfusion: age over 75 years (odds ratio [OR] 2.61 [1.38-4.91], p=0.003), intertrochanteric fractures (OR 2.97 [1.10-7.96], p=0.031), and initial hematocrit <30.0% (OR 55.61 [16.26-190.15], p<0.001). Patients with an initial hematocrit level ≥36.0% had a transfusion rate of 16.10%, while those with a level above 43.2% did not require transfusion. The mean hematocrit level decrease was 1.73±0.46% in extracapsular fractures and 0.74±2.65% in intracapsular fractures.
Conclusions: Elderly patients with hip fracture with an initial hematocrit level of <36% should be considered for serial preoperative blood testing and intraoperative blood reservation. For those with a hematocrit level 36.0–43% may not require preoperative blood testing and reservation, based on the physician’s discretion, and levels >43% generally do not necessitate preoperative blood testing or reservation.
Metrics
References
Simunovic N, Devereaux PJ, Sprague S, et al. Effect of early surgery after hip fracture on mortality and complications: systematic review and meta-analysis. CMAJ 2010;182:1609-16. DOI: https://doi.org/10.1503/cmaj.092220
van Rijckevorsel VA, de Jong L, Verhofstad MH, et al. Influence of time to surgery on clinical outcomes in elderly hip fracture patients: an assessment of surgical postponement due to non-medical reasons. Bone Joint J 2022;104:1369-78. DOI: https://doi.org/10.1302/0301-620X.104B12.BJJ-2022-0172.R2
Smith GH, Tsang J, Molyneux SG, et al. The hidden blood loss after hip fracture. Injury 2011;42:133-5. DOI: https://doi.org/10.1016/j.injury.2010.02.015
Wu J-Z, Liu P-C, Ge W, Cai M. A prospective study about the preoperative total blood loss in older people with hip fracture. Clin Interv Aging 2016;11:1539-43. DOI: https://doi.org/10.2147/CIA.S120526
Desai SJ, Wood KS, Marsh J, et al. Factors affecting transfusion requirement after hip fracture: Can we reduce the need for blood? Can J Surg 2014;57:342-8. DOI: https://doi.org/10.1503/cjs.030413
Arshi A, Lai WC, Iglesias BC, et al. Blood transfusion rates and predictors following geriatric hip fracture surgery. Hip Int 2020;31:272-9. DOI: https://doi.org/10.1177/1120700019897878
Jang SY, Cha YH, Yoo JI, et al. Blood transfusion for elderly patients with hip fracture: a nationwide cohort study. J Korean Med Sci 2020;35:e313. DOI: https://doi.org/10.3346/jkms.2020.35.e313
Greenhalgh MS, Gowers BT, Iyengar KP, et al. Blood transfusions and hip fracture mortality - A retrospective cohort study. J Clin Orthop Trauma 2021;21:101506. DOI: https://doi.org/10.1016/j.jcot.2021.101506
Bian FC, Cheng XK, An YS. Preoperative risk factors for postoperative blood transfusion after hip fracture surgery: Establishment of a nomogram. J Orthop Surg Res 2021;16. DOI: https://doi.org/10.1186/s13018-021-02557-5
Madsen CM, Jørgensen HL, Norgaard A, et al. Preoperative factors associated with red blood cell transfusion in hip fracture patients. Arch Orthop Trauma Surg 2013;134:375-82. DOI: https://doi.org/10.1007/s00402-013-1906-3
Loftus TJ, Brakenridge SC, Murphy TW, et al. Anemia and blood transfusion in elderly trauma patients. J Surg Res 2018;229:288-93. DOI: https://doi.org/10.1016/j.jss.2018.04.021
Morris R, Rethnam U, Russ B, et al. Assessing the impact of fracture pattern on transfusion requirements in hip fractures. Eur J Trauma Emerg Surg 2016;43:337–42. DOI: https://doi.org/10.1007/s00068-016-0655-8
Harper KD, Navo P, Ramsey F, et al. “Hidden” preoperative blood loss with extracapsular versus intracapsular hip fractures: what is the difference?. eriatr Orthop Surg Rehabil 2017;8:202-7. DOI: https://doi.org/10.1177/2151458517729615
Konda SR, Parola R, Perskin CR, et al. Transfusion thresholds can be safely lowered in the hip fracture patient: A consecutive series of 1,496 patients. J Am Acad Orthop Surg 2023;31:349-56. DOI: https://doi.org/10.5435/JAAOS-D-22-00582
Brunskill SJ, Millette SL, Shokoohi A, et al. Red blood cell transfusion for people undergoing hip fracture surgery. Cochrane Database Syst Rev201;2015:CD009699. DOI: https://doi.org/10.1002/14651858.CD009699.pub2
Griffiths R, Babu S, Dixon P, et al. Guideline for the management of hip fractures 2020: Guideline by the Association of Anaesthetists. Anaesthesia 2021;76:225-37. DOI: https://doi.org/10.1111/anae.15291
Mattisson L, Lapidus LJ, Enocson A. What is the influence of a delay to surgery >24 hours on the rate of red blood cell transfusion in elderly patients with intertrochanteric or subtrochanteric hip fractures treated with cephalomedullary nails? J Orthop Trauma 2018;32:403-7. DOI: https://doi.org/10.1097/BOT.0000000000001183
Hou G, Zhou F, Tian Y, et al. Predicting the need for blood transfusions in elderly patients with pertrochanteric femoral fractures. Injury 2014;45:1932-7. DOI: https://doi.org/10.1016/j.injury.2014.08.033
Konda SR, Perskin CR, Parola R, et al. Trauma risk score also predicts blood transfusion requirements in hip fracture patients. Geriatr Orthop Surg Rehabil 2021;12:21514593211038387. DOI: https://doi.org/10.1177/21514593211038387
Tarazona-Santabalbina FJ, Ojeda-Thies C, Figueroa Rodríguez J, et al. Orthogeriatric management: improvements in outcomes during hospital admission due to hip fracture. Int J Environ Res Public Health 2021;18:3049. DOI: https://doi.org/10.3390/ijerph18063049
Patel PA, Wyrobek JA, Butwick AJ, et al. Update on applications and limitations of perioperative tranexamic acid. Anesth Analg 2022;135:460-73. DOI: https://doi.org/10.1213/ANE.0000000000006039
Deeruksa L, Sanchaisuriya K. Anemia in the elderly in northeastern Thailand: a community-based study investigating prevalence, contributing factors, and hematologic features. Acta Haematol 2017;138:96-102. DOI: https://doi.org/10.1159/000478771
Singsanan S, Chonanant C, Prakobkaew N. Prevalence of anemia, iron deficiency and thalassemia among elder population [Internet]. Burapha University; 2018 [cited 2025 May 20]. Available from https://digital_collect.lib.buu.ac.th/research/2563_243.pdf.
Budair B, Ahmed U, Hodson J, et al. Are we all guilty of under-estimating intra-operative blood loss during hip fracture surgery? J Orthop 2017;14:81-4. DOI: https://doi.org/10.1016/j.jor.2016.10.019
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 The Royal College of Orthopaedic Surgeons of Thailand

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.